The incisions used for Breast Augmentation usually heal well. Carefully planned incision placement pre-operatively, meticulous intra-operative care and post-operative scar massage and topical treatments all contribute to good outcomes. As a result the vast majority of Breast Enhancement patients are happy with the appearance and location of their scars. A small percentage of scars, however, heal raised or widespread, and may remain irritated and at times itchy. These types of scars may benefit from Breast Scar Revision.
Breast Lift and Breast Reduction incisions also usually heal well. Unlike Breast Augmentation incisions, the incisions for these procedures are more than just opening through which to place a Breast Implant. The incisions for Breast Lift and Breast Reduction are used to remove excess skin, lift, firm and change the shape of the breasts. As a result, the incisions are longer and in more exposed locations. Breast Scar Revision can often improve results by not only improving the look of the scar, but sometimes Breast Scar Revision will also change the location and shape of the scars to enhance appearance and symmetry.
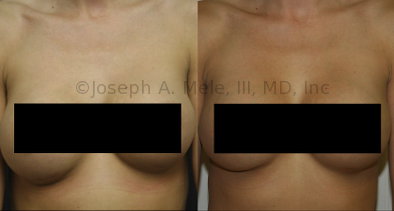
Breast Implant Revision Before and After Photos





.jpg)




.jpg)






.jpg)




.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)

.jpg)
.jpg)
.jpg)
.jpg)
What Makes a Good Scar?
A good scar matches the surrounding skin. It is smooth, flat, thin and matches the surrounding tissues in color and texture. It is painless, soft and does not restrict motion or cause distortion of adjacent structures.
The ideal Scar Revision would remodel a scar into a smooth surface, resembling the surrounding skin in all respects. If this were possible, a scar would be virtually invisible. Unfortunately, a scar cannot be completely erased. By reducing those qualities that make the scar apparent, a scar can often be improved.
The Goals of Scar Revision
The goal of Scar Revision is to make the scar blend in. By getting as close as possible to the ideal result, the scar is made less noticeable. Here are some as some qualities that plastic surgeons try to create in the revised scar:
- A fine line scar (narrow is best)
- Falling within, or parallel to, naturally occurring lines, wrinkles, contour junctions
- Oriented along the resting skin tension lines (perpendicular to the underlying muscle fibers)
- Free of contour irregularities (no lumps or depressions)
- Without abnormal pigmentation (not too dark, not too light)
- Void of contractures or distortions of the surrounding tissue (not too tight)
When planning Scar Revision surgery, it is important to determine what makes the scar apparent, and focus on the methods most likely to mute these attributes. For example, if a scar is raised, silicone gel sheeting can help to flatten it. However, using silicone gel sheeting on a depressed scar is not likely to help. The correct tool for the job can only be selected after deciding what the job is.
How Does Scar Revision Help?
There are many different ways to treat a scar, and most help in at least one of the following ways:
- Improving the direction of the scar.
- Decreasing the width of the scar.
- Dividing the scar into smaller segments.
- Correcting misalignment or distortion of adjacent tissues.
- Improving surface irregularities.
- Improving pigment discrepancies.
Scar Revision Evaluation
The evaluation of a scar encompasses the following ten points, the first and last may be the most important.
1 – Time Since Injury
Scar Revision is usually performed on mature scars. Depending on your age, this normally requires one to two years of healing. In general, the younger you are, the longer it takes for a scar to mature.
A mature scar has entered the “resting” phase of healing, and can be recognized as a soft, pliable scar in which the redness has faded. Sometimes the maturation process can be accelerated with the use of pressure, massage, steroids or silicone gel sheeting.
There are times when waiting will not help; however, this is the exception rather than the rule. Examples include cases of gross misalignment, i.e. a step-off at the border of a lip, or an injury causing severe distortion, i.e. exposure of an eye or inability to straighten a joint.
2 – Nature of the Injury
The type of injury and the mechanism of injury can influence the treatment. Whether an injury is from a surgical scar or an animal bite is important in planning a revision. A carefully planed operative incision is more likely to heal in an optimal fashion, and as a result, is less likely to require a scar revision. An injury which is not planned, such as an animal bite, or a wound which was infected, tends to give a worse scar and will be more likely to require from revision.
3 – Location of the Injury
Scars of the head and face, in general, respond more favorably to revisions. Areas below the clavicle can often still be improved; however, they are less likely to improve. A triangle on the chest, formed by the shoulders and the lowest portion of the sternum, is a “Danger Zone”. The thicker skin in this area, the weight of the skin (and breasts) and the pull of the underlying muscles, can produce a widespread and darkened scar, even under otherwise ideal conditions.
The orientation (direction) of the scar can also be important. When possible, the scar is positioned perpendicular to the underlying muscle to provide a narrower scar and improve its appearance. Wrinkles tend to run in the same direction, and these may also disguise the scar. Scars placed in the inframammary fold (below the breast), are perpendicular to the underlying muscles, have the weight of the skin compressing the scar and are hidden in the shadow of the breast to help with healing and appearance.
4 – Age of the Patient
Older people tend to require scar revisions less often than younger ones. Younger people heal more exuberantly, and over a longer period of time. This leads to a higher incidence of hypertrophic (excess) scars in the young. Because of this exuberant wound healing, it is also necessary to delay Scar Revision longer after the initial injury if you are younger.
5 – Ethnicity
The darker the hair, skin, and eyes, the more likely a noticeable scar is to form. Wounds in darker skin tend to be darker, wider, lumpier and more problematic than wounds in lighter skin. The biochemical reasons for this are still largely unknown, and there are well documented exceptions to this rule. It is due in part to innate differences in the healing, and in part to how the scar appears as light reflects off of it. This is explained further below.
6 – Skin Tone and Light Effects
For someone with fair skin, light reflecting off a scar may go unnoticed, but the same scar in darker pigmented skin will be easily spotted. What catches the eye is the difference in brightness between the reflected light, and the surrounding skinÕs color.
7 – Healing of Previous Injuries
Healing varies from area to area. A previous injury can be an indicator of what type of scar to expect. If nearby scars are all widespread, raised and darkly pigmented, then chances are higher that a revision will also be widespread, raised and darkly pigmented.
8 – The Nature of the Scar
As a simplification, scars can be separated into four groups: a fine line scar (the desired result, flat and thin); a widespread scar (flat but wide); a hypertrophic scar (raised and wide); and a keloid scar (raised and extending outside the original zone of injury). The more the original scar is like a keloid scar, the less likely a revision of this scar will result in a fine line scar. Sometimes, the first sign of someone being a keloid former is when the ears are pierced. A hard knot will form at the piercing that will continue to grow.
9 – Loss of Skin
If a significant amount of skin is lost at the time of the original injury, like with a Breast Lift or Breast Reduction, then closure of that wound may result in increased tension at the site of repair. Tension is the enemy of fine line scars. The greater the tension, the higher the risk of a wide scar.
10 – Perceptions and Expectations
This may be the most important part of the evaluation. If your expectation is that your scar will become completely invisible, you will be disappointed, no matter how much improvement is achieved. However, if you understand what makes the scar more obvious, and understand which of these features can be expected to improve (and conversely which will not improve) then an informed decision can be made. If your decision to proceed with the revision is based on realistic goals, then you will achieve greater satisfaction with the results of Scar Revision. A scar will always remain a scar, but if we improve a scar’s appearance, we can make it less noticeable and distracting.
Breast Augmentation Scar Revision Before and After Photos

Above are breast scar revision before and after photos of periareolar scars.
- Before: The upper picture is before the breast augmentation scar revision and reveals pale, widespread scars, which were poorly placed. The incisions were made within the areola, instead of along the margins. The peripheral dark areola skin only helps to define the white scars and makes them more apparent.
- After: The lower photo is after breast augmentation scar revision. The wide, white scar was excised, and the new scar was placed more peripherally, curving along the edge of the areola. The edges were carefully reapproximated in layers, reinforcing the skin margins and supporting the closure from inside out. Minimizing the tension across the repair reduces the tendency for the scar to spread. The result is a fine white scar, and a much more cosmetically acceptable scar. By placing the scar along the edge of the areola, the scar is camouflaged. This method works well for both light and dark scars. Lighter scars will hide in the skin, and darker scars will hide in the areola.
Scar Revision Treatment Options
So how can hypertrophic and keloid scars be improved? What options are available to treat unsatisfactory scars? Here are some of the different Scar Treatments utilized.
Excision and Primary Closure
This is one of the most commonly used Scar Revision techniques. It often involves making a lens-shaped excision, to remove the scar and a small amount of the surrounding normal skin, then careful re-closure of the new wound. Wide undermining may be employed, to reduce the tension across the repair.
Z-Plasty or W-Plasty
These are techniques for rearranging the scar. Their names are derived from the pattern of the resultant scar. Z-plasty may be used to lengthen a scar if it is pulling too tightly, or to change the direction of a scar, to make it less conspicuous. These are useful techniques for improving tight mastectomy scars. Both can be used to align scars with an existing wrinkle or landmark and make the scars less noticeable.
Layered Closure
Deep, dissolvable sutures (stitches) are used to bring the edges of the skin together. These do not need to be removed. Thinner sutures are used for the fine tailoring, to line-up the two edges of the wound. The superficial sutures are not always dissolvable. Non-dissolvable sutures need to be removed, but they also decrease the amount of inflammation at the surface, where the scar is forming. How long before removal depends on the location and nature of the scar. For example, sutures on the face often can be removed in less than a week, on the breast about a week, while those on the sole of the foot may need to stay for two weeks.
Buried Dermal Flap
Sometimes the scar is concave (indented). When this happens, something is needed to fill in the missing volume beneath scar. Available options include: using a portion of the original scar as a filler, imbricating the deeper layers of the surrounding normal skin for bulk, or occasionally, an artificial filler can be used. These methods of adding volume beneath the repair bring the level of the revised scar up to that of the surrounding skin.
“Dog Ears”
Occasionally, a discrepancy in the length or positioning of the sides of a wound results in a raised points at the ends of the scar. These are referred to as “Dog Ears”, perhaps because they stand up and are often found in pairs. Revision of a “dog ear” requires lengthening or changing the direction of the original scar to smooth out the ends. This can occur at the inner or outer end of a Breast Lift or Breast Reduction scar due to making the scar too short.
Skin Graft and Flaps
Skin grafts and flaps are not needed for most scar revisions. They are reserved for larger or wider scars, such as burn scars, that cover a large area. Sometimes scars are too large to simply excise and close. More complicated techniques like tissue expansion, composite flaps and microvascular transplantation (free flaps), have evolved to move “normal” skin into the proper position. These types of techniques are used more often for Breast Reconstruction, and are rarely necessary for Cosmetic Breast Surgery
Dermabrasion
This is the same technique use for treating wrinkles, and is useful for surface irregularities, or scars with obvious shadows or highlights. Dermabrasion can be performed either shortly after a scar revision, or after the scar has matured. Dermabrasion appears to work better if used at 4 months rather than 8 months after the revision. This has led some Plastic Surgeons to use dermabrasion at the time of the scar revision.
Lasers (Laserbrasion)
There are many types of lasers. The CO2 and Erbium lasers work very similarly to dermabrasion. They remove the outer layers of the skin, and can be used to take down high points.
The blue-green Argon and flashlamp pumped dye lasers, are more selectively absorbed by blood vessels and skin pigments, and can be used to treat red, purple or pigmented scars.
Pressure and Massage
These modalities can be used alone or in conjunction with the methods listed above. Pressure and massage cause realignment of the fibers in the scar and surrounding skin, and can dramatically flatten and smooth raised scars. This may be why Vitamin E works – the Vitamin E oil remains on the surface, touching only the dead surface skin cells; however, the continuing replication ensures adequate scar massage is performed.
Gel Sheeting
Both Mineral Oil and Silicone Gel impregnated sheeting seem to decrease the time needed for a scar to soften and mature, and as a result may lead to the accelerated formation of smoother scars. Like massage, sheeting can also be used alone or with other treatments. The drawbacks include the possibility of dermatitis (irritation of the skin), foliculitis (irritation or infection of the hairs) or scar ulceration. The sheets must be worn 12-18 hours a day and treatment may be needed for as long as 18 months.
Topical Silicone Gel
Silicone Gel (Biodermis, Kelocote) also comes as topical gel that is applied twice a day. It is easier to use than gel sheeting, but may not always give the same results. The silicone gel softens the scar and helps reduce the redness seen early in scar healing. Like gel sheeting. the drawbacks include the possibility of skin or scar irritation.
Steroids
Occasionally injectable steroids are used to slow scar formation. Drawbacks include the possibility of lightening the color of the surrounding normal skin, and tissue atrophy creating a widespread and depressed scar. If steroids are used at the time of repair/revision, the wound will require extra support. Frequently this means sutures must be left in longer.
Bleaching agents
Topical skin bleaches, such as Hydroquinone and Kojic Acid, can sometimes fade a darker scar, or even prevent its occurrence. It takes several months for the effects to be seen and longer to reach optimal results, so compliance is an issue. Bleaching agents can be used separately or with a surgical scar revision.
Scar Revision Anesthesia
Scar Revision can be performed under both general and local anesthesia. Local anesthesia is usually all that is necessary to perform most scar revisions. Occasionally for larger scars, or younger patients, regional or general anesthetic is needed. The type of anesthesia needed will be discussed prior to surgery.
Often epinephrine (adrenaline) is added to the local anesthetic, to minimize any bleeding. This allows the Plastic Surgeon to see better when they are repairing the incision. Epinephrine may temporarily give the sensation that your heart is racing, but this passes quickly. For patients with cardiac problems, additional precautions may be necessary, or the epinephrine may be left out entirely.
Scar Revision Risks
For scar revision, as with any surgical procedure, there are potential risks that accompany the potential benefits. Here are some of the more common risks:
Hematoma/Seroma Formation
Fluid tends to collect in the operative site. A small amount is normal. If a large collection of fluid accumulates, then it may need to be removed. Usually this is easily treated in the office by aspiration; occasionally the wound may need to opened temporarily or a drain may need to be placed. It is important to remove large fluid collections as these may become infected or put too much tension on the wound.
Infection
As with any scrape or cut, an operative site can become infected. For clean cases, antibiotics are not needed. For cases that are potentially contaminated, a dose of antibiotics can be given just before surgery to minimize this risk. Occasionally, antibiotics may be continued for several days after surgery. Even with precautions, an infection can occur, and signs of infection including: redness, pain, swelling, discharge from the wound or fever, should be promptly reported.
Dehiscence (Reopening) of the Wound
This can occur if too much tension is placed on the wound, before it has fully healed. If dehiscence occurs the wound must be cleansed, and if appropriate, sutured again. If the dehiscence is due to infection, delayed primary closure or healing by secondary intention may be recommended.
Milia (Whiteheads)
Milia frequently occur around scars, and are almost always seen with dermabrasion and ablative laser treatments. Milia represent blocked glands, or trapped surface skin cells. They can be treated in the office, by gently unroofing them. Once adequately treated, they tend not to recur.
Hyperpigmentation/Hypopigmentation
The resultant scar can become darker (hyperpigmented) or lighter (hypopigmented) compared to the surrounding skin. Too much pigmentation can occur as a direct result of exposure to the sun. A sunblock, no less than SPF 15, is recommended until the new scar is fully matured (approximately one year). If the scar is under clothing, this is less of a problem. If the scar is on the face or neck, a hat is recommended. Skin bleaches are also available to lighten a darkening scar. A light scar on dark skin is more difficult to treat, but options such as make-up and tattooing can be utilized.
Recurrence
Despite the most meticulous, careful repair, there is always the possibility that another unsatisfactory scar may result. It may even look worse! This is why a careful dialogue between you and your plastic surgeon is critical. You need to know the chances for improvement, and which aspects of the scar are likely to improve.